Nipah Virus: Seven Vital Things You Should Understand
India is currently grappling with a Nipah virus outbreak, and it’s crucial to grasp the key facts about this virus and the risks it poses. Here, we break down seven important insights about Nipah virus in a more accessible manner.
1. A Recent Discovery Nipah virus came into the spotlight in March 1999 when it was first identified in a patient from Sungai Nipah, a village in Malaysia. This virus, previously unknown, belongs to the same family as measles and mumps. It got its name from the place where it was first found. It later caused a severe illness in Malaysia and Singapore.
2. Spreading to New Areas Since its discovery, Nipah virus has not stayed put. Outbreaks have occurred in different parts of the world, including Bangladesh, India, and the Philippines. Bangladesh saw frequent outbreaks from 2001 to 2013, mainly linked to contact with fruit bats. The numbers may sound alarming, but globally, they are relatively small, with 634 cases and 376 deaths reported before the current outbreak in India.
3. Increasing Fatality Rates Though we can’t say for sure if Nipah virus is becoming deadlier, recent outbreaks in Bangladesh and India have shown higher fatality rates compared to earlier outbreaks in Malaysia and the Philippines. The 2018 outbreak in Kerala, India, had a shocking fatality rate of 94.4%. Different strains of Nipah virus exist, with varying levels of severity. The Bangladesh strain, which causes muscle weakness, cough, and breathing difficulties, can even spread directly from one person to another.
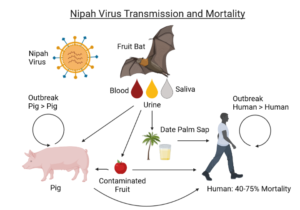
4. Multiple Ways of Infection Nipah virus mainly targets fruit bats as its natural hosts. However, it can infect humans and other animals through various routes. People often get exposed to the virus by consuming things tainted with bat urine, saliva, or droppings. The problem is, bat roosting sites are often close to human homes and fruit trees. Additionally, bat guano, used as fertilizer, can put agricultural workers at risk. The virus can also spread through contact with infected animals like pigs and horses.
5. Passing the Virus Among Humans Research shows that Nipah virus can spread from one person to another through direct contact with infected individuals and their bodily fluids, including urine, blood, and respiratory droplets. We’ve seen this happen in healthcare settings, where healthcare workers, caregivers, and visitors have been infected. There have also been cases within households.
6. Controlling Outbreaks To prevent Nipah outbreaks, it’s crucial to minimize contact with bats and follow strict hygiene practices. This includes washing fruits and veggies before eating them, practicing good hand hygiene after handling produce, and properly cleaning containers used for collecting palm sap. Culling infected animals, like pigs, has proven effective. Reducing human-to-human transmission risks involves practices like frequent handwashing, avoiding sharing food or bedding with infected individuals, and using protective gear when handling deceased Nipah patients. The 2018 outbreak in Kerala demonstrated that effective measures like contact tracing, isolation, and improved hospital infection control can bring an outbreak under control.
7. Vaccine Development While there are no approved vaccines or treatments for Nipah virus in humans at the moment, there’s promising progress in vaccine development. Several vaccines are in clinical trials, including ones based on mRNA and vesicular stomatitis virus. Researchers in Bangladesh are studying Nipah survivors to gain insights into the virus and support vaccine development.
In summary, Nipah virus requires vigilance, but with increased awareness, good hygiene practices, and ongoing research, we can better protect ourselves against this challenging virus.

